 |
| Menopause in Women: Symptoms and Causes |
Menopause is a natural biological
process. But the physical symptoms, such as hot flashes, and emotional symptoms
of menopause may disrupt your sleep, lower your energy or affect emotional
health. There are many effective treatments available, from lifestyle
adjustments to hormone therapy.
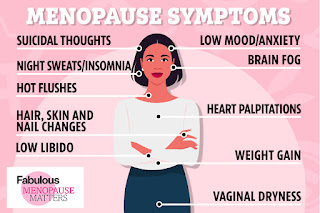
Symptoms
In the months or years leading up to
menopause (perimenopause), you might experience these signs and symptoms:
- Irregular
periods
- Vaginal
dryness
- Hot
flashes
- Chills
- Night
sweats
- Sleep
problems
- Mood
changes
- Weight
gain and slowed metabolism
- Thinning
hair and dry skin
- Loss
of breast fullness
Signs and symptoms, including changes
in menstruation, can vary among women. Most likely, you'll experience some
irregularity in your periods before they end.
Skipping periods during perimenopause
is common and expected. Often, menstrual periods will skip a month and return,
or skip several months and then start monthly cycles again for a few months.
Periods also tend to happen on shorter cycles, so they are closer together.
Despite irregular periods, pregnancy is possible. If you've skipped a period
but aren't sure you've started the menopausal transition, consider a pregnancy
test.
When to see a doctor
Keep up with regular visits with your doctor for
preventive health care and any medical concerns. Continue getting these
appointments during and after menopause.
Preventive health care as you age may include
recommended health screening tests, such as colonoscopy, mammography, and
triglyceride screening. Your doctor might recommend other tests and exams, too,
including thyroid testing if suggested by your history, and breast and pelvic
exams.
Always seek medical advice if you have bleeding
from your lady parts after menopause.
Causes
Menopause can result from:
Naturally declining reproductive hormones.
As you approach your late 30s, your ovaries start making less estrogen and progesterone — the hormones that regulate menstruation — and your fertility declines.In your 40s, your menstrual periods may become longer or
shorter, heavier or lighter, and more or less frequent, until eventually — on
average, by age 51 — your ovaries stop releasing eggs, and you have no more
periods.
Surgery that removes the ovaries (oophorectomy).
Your ovaries produce hormones, including estrogen and progesterone, that regulate the menstrual cycle. Surgery to remove your ovaries causes immediate menopause. Your periods stop, and you're likely to have hot flashes and experience other menopausal signs and symptoms. Signs and symptoms can be severe, as hormonal changes occur abruptly rather than gradually over several years.Surgery that removes your uterus but not your ovaries
(hysterectomy) usually doesn't cause immediate menopause. Although you no
longer have periods, your ovaries still release eggs and produce estrogen and
progesterone.
Chemotherapy and radiation therapy.
These cancer therapies can induce menopause, causing symptoms such as hot flashes during or shortly after the course of treatment. The halt to menstruation (and fertility) is not always permanent following chemotherapy, so birth control measures may still be desired. Radiation therapy only affects ovarian function if radiation is directed at the ovaries. Radiation therapy on other parts of the body, such as breast tissue or the head and neck, won't affect menopause.Primary ovarian insufficiency.
About 1% of women experience menopause before age 40 (premature menopause). Premature menopause may result from the failure of your ovaries to produce normal levels of reproductive hormones (primary ovarian insufficiency), which can stem from genetic factors or autoimmune disease. But often no cause of premature menopause can be found. For these women, hormone therapy is typically recommended at least until the natural age of menopause in order to protect the brain, heart, and bones.
Complications
After menopause, your risk of certain
medical conditions increases. Examples include:
Heart and blood vessel (cardiovascular) disease.
When your estrogen levels decline, your risk of cardiovascular disease increases. Heart disease is the leading cause of death in women as well as in men. So it's important to get regular exercise, eat a healthy diet and maintain a normal weight. Ask your doctor for advice on how to protect your heart, such as how to reduce your cholesterol or blood pressure if it's too high.Osteoporosis.
This condition causes bones to become brittle and weak, leading to an increased risk of fractures. During the first few years after menopause, you may lose bone density at a rapid rate, increasing your risk of osteoporosis. Postmenopausal women with osteoporosis are especially susceptible to fractures of their spine, hips, and wrists.Urinary incontinence.
As the tissues of your vagina and urethra lose elasticity, you may experience frequent, sudden, strong urges to urinate, followed by an involuntary loss of urine (urge incontinence), or the loss of urine with coughing, laughing, or lifting (stress incontinence). You may have urinary tract infections more often.Strengthening pelvic floor muscles with
Kegel exercises and using topical vaginal estrogen may help relieve symptoms
of incontinence. Hormone therapy may also be an effective treatment option for
menopausal urinary tract and vaginal changes that can result in urinary
incontinence.
Sexual function.
Vaginal dryness from decreased moisture production and loss of elasticity can cause discomfort and slight bleeding during sexual intercourse. Also, decreased sensation may reduce your desire for sexual activity (libido).Water-based vaginal moisturizers and
lubricants may help. If a vaginal lubricant isn't enough, many women benefit
from the use of local vaginal estrogen treatment, available as a vaginal cream,
tablet, or ring.
Weight gain.
Many women gain weight during the menopausal transition and after menopause, because metabolism slows. You may need to eat less and exercise more, just to maintain your current weight.
Diagnosis
Signs and symptoms of menopause are
usually enough to tell most women that they've started the menopausal
transition. If you have concerns about irregular periods or hot flashes, talk
with your doctor. In some cases, further evaluation may be recommended.
Tests typically aren't needed to
diagnose menopause. But under certain circumstances, your doctor may recommend
blood tests to check your level of:
- Follicle-stimulating
hormone (FSH) and estrogen (estradiol), because your FSH levels
increase and estradiol levels decrease as menopause occurs
- Thyroid-stimulating
hormone (TSH), because an underactive thyroid (hypothyroidism) can cause
symptoms similar to those of menopause
Over-the-counter home tests to
check FSH levels in your urine are available. The tests could tell
you whether you have elevated FSH levels and might be in
perimenopause or menopause. But, since FSH levels rise and fall
during the course of your menstrual cycle, home FSH tests can't
really tell you whether or not you're definitely in a stage of menopause.
Treatment
Menopause requires no medical
treatment. Instead, treatments focus on relieving your signs and symptoms and
preventing or managing chronic conditions that may occur with aging. Treatments
may include:
Hormone therapy.
Estrogen therapy is the most effective treatment option for relieving menopausal hot flashes. Depending on your personal and family medical history, your doctor may recommend estrogen in the lowest dose and the shortest time frame needed to provide symptom relief for you. If you still have your uterus, you'll need progestin in addition to estrogen. Estrogen also helps prevent bone loss. Long-term use of hormone therapy may have some cardiovascular and breast cancer risks, but starting hormones around the time of menopause has shown benefits for some women. Talk to your doctor about the benefits and risks of hormone therapy and whether it's a safe choice for you.Vaginal estrogen.
To relieve vaginal dryness, estrogen can be administered directly to lady parts using a vaginal cream, tablet, or ring. This treatment releases just a small amount of estrogen, which is absorbed by the vaginal tissues. It can help relieve vaginal dryness, discomfort with intercourse, and some urinary symptoms.Low-dose antidepressants.
Certain antidepressants related to the class of drugs called selective serotonin reuptake inhibitors (SSRIs) may decrease menopausal hot flashes. A low-dose antidepressant for the management of hot flashes may be useful for women who can't take estrogen for health reasons or for women who need an antidepressant for a mood disorder.Gabapentin (Gralise, Horizant, Neurontin).
Gabapentin is approved to treat seizures, but it has also been shown to help reduce hot flashes. This drug is useful in women who can't use estrogen therapy and in those who also have nighttime hot flashes.Clonidine (Catapres, Kapvay).
Clonidine, a pill or patch typically used to treat high blood pressure, might provide some relief from hot flashes.Medications to prevent or treat osteoporosis.
Depending on individual needs, doctors may recommend medication to prevent or treat osteoporosis. Several medications are available that help reduces bone loss and the risk of fractures. Your doctor might prescribe vitamin D supplements to help strengthen bones.Before deciding on any form of
treatment, talk with your doctor about your options and the risks and benefits
involved with each. Review your options yearly, as your needs and treatment
options may change.
Lifestyle and home remedies
Fortunately, many of the signs and
symptoms associated with menopause are temporary. Take these steps to help
reduce or prevent their effects:
- Cool hot flashes. Dress
in layers have a cold glass of water, or go somewhere cooler. Try to
pinpoint what triggers your hot flashes. For many women, triggers may
include hot beverages, caffeine, spicy foods, alcohol, stress, hot weather, and even a warm room.
- Decrease vaginal discomfort. Try an
over-the-counter, water-based vaginal lubricant (Astroglide, K-Y jelly,
Sliquid, others) or a silicone-based lubricant or moisturizer (Replens,
K-Y Liquibeads, Sliquid, others).
You might consider choosing a product
that doesn't contain glycerin, which can cause burning or irritation if you're
sensitive to that chemical. Staying sexually active also helps with vaginal
discomfort by increasing blood flow to the lady parts.
- Get enough sleep. Avoid
caffeine, which can make it hard to get to sleep, and avoid drinking too
much alcohol, which can interrupt sleep. Exercise during the day, although
not right before bedtime. If hot flashes disturb your sleep, you may need
to find a way to manage them before you can get adequate rest.
- Practice relaxation techniques. Techniques
such as deep breathing, paced breathing, guided imagery, massage, and
progressive muscle relaxation may help with menopausal symptoms. You can
find a number of books and online offerings that show different relaxation
exercises.
- Strengthen your pelvic floor. Pelvic
floor muscle exercises, called Kegel exercises, can improve some forms of
urinary incontinence.
- Eat a balanced diet. Include
a variety of fruits, vegetables, and whole grains. Limit saturated fats,
oils, and sugars. Ask your provider if you need calcium or vitamin D
supplements to help meet daily requirements.
- Don't smoke. Smoking
increases your risk of heart disease, stroke, osteoporosis, cancer, and a
range of other health problems. It may also increase hot flashes and bring
on earlier menopause.
- Exercise regularly. Get
regular physical activity or exercise on most days to help protect against
heart disease, diabetes, osteoporosis, and other conditions associated with
aging.
Alternative medicine
Many approaches have been promoted as aids in managing the symptoms of menopause, but few of them have scientific evidence to back up the claims. Some complementary and alternative treatments that have been or are being studied include:
Plant estrogens (phytoestrogens).
These estrogens occur naturally in certain foods. There are two main types of phytoestrogens — isoflavones and lignans. Isoflavones are found in soybeans, lentils, chickpeas, and other legumes. Lignans occur in flaxseed, whole grains, and some fruits and vegetables.Whether the estrogens in these foods
can relieve hot flashes and other menopausal symptoms remains to be proven, but
most studies have found them ineffective. Isoflavones have some weak
estrogen-like effects, so if you've had breast cancer, talk to your doctor
before supplementing your diet with isoflavone pills.
The herb sage is thought to contain compounds with estrogen-like effects, and there's good evidence that it can effectively manage menopause symptoms. The herb and its oils should be avoided in people who have an allergy to sage, and in pregnant or breastfeeding women. Use carefully in people with high blood pressure or epilepsy
Bioidentical hormones.
These hormones come from plant sources. The term "bioidentical" implies the hormones in the product are chemically identical to those your body produces. There are some commercially available bioidentical hormones approved by the Food and Drug Administration (FDA). But many preparations are compounded — mixed in a pharmacy according to a doctor's prescription — and aren't regulated by the FDA, so quality and risks could vary. There's no scientific evidence that bioidentical hormones work any better than traditional hormone therapy in easing menopause symptoms. There's also no evidence that they're any less risky than traditional hormone therapy.Black cohosh.
Black cohosh has been popular among many women with menopausal symptoms. But there's little evidence that black cohosh is effective, and the supplement can be harmful to the liver and may be unsafe for women with a history of breast cancer.Yoga.
Acupuncture.
Hypnosis.
You may have heard of or tried other
dietary supplements, such as red clover, kava, dong Quai, DHEA, evening
primrose oil, and wild yam (natural progesterone cream). Scientific evidence on
effectiveness is lacking, and some of these products may be harmful.
Talk with your doctor before taking any
herbal or dietary supplements for menopausal symptoms. The FDA does
not regulate herbal products, and some can be dangerous or interact with other
medications you take, putting your health at risk.
( Keywords )



Post a Comment