 |
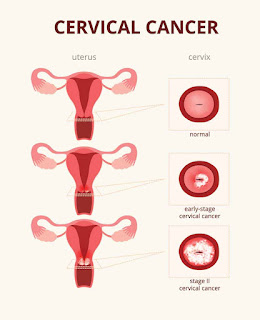
| Cervical cancer Symptoms and causes |
Various strains of the human
papillomavirus (HPV), a sexually transmitted infection, play a role in causing
most cervical cancer.
When exposed to HPV, the body's
immune system typically prevents the virus from doing harm. In a small
percentage of people, however, the virus survives for years, contributing to
the process that causes some cervical cells to become cancer cells.
You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection.
Symptoms
Early-stage cervical cancer generally
produces no signs or symptoms.
Signs and symptoms of more-advanced
cervical cancer include:
- Vaginal
bleeding after intercourse, between periods, or after menopause
- Watery,
bloody vaginal discharge that may be heavy and have a foul odor
- Pelvic
pain or pain during intercourse
When to see a doctor
Make an appointment with your doctor if you have any signs or symptoms that concern you.
Causes
Cervical cancer begins when healthy cells in the cervix develop
changes (mutations) in their DNA. A cell's DNA contains the
instructions that tell a cell what to do.
Healthy cells grow and multiply at a set rate, eventually dying
at a set time. The mutations tell the cells to grow and multiply out of
control, and they don't die. The accumulating abnormal cells form a mass
(tumor). Cancer cells invade nearby tissues and can break off from a tumor to
spread (metastasize) elsewhere in the body.
It isn't clear what causes cervical cancer, but HPV certainly plays a role. HPV is very common, and most people
with the virus never develop cancer. This means other factors — such as your
environment or your lifestyle choices — also determine whether you'll develop
cervical cancer.
Types of cervical cancer
The type of cervical cancer that you have help determine your
prognosis and treatment. The main types of cervical cancer are:
Squamous cell carcinoma.
This type of cervical cancer begins in the thin, flat cells (squamous cells) lining the outer part of the cervix, which projects into the lady parts. Most cervical cancers are squamous cell carcinomas.Adenocarcinoma.
Sometimes, both types of cells are involved in cervical cancer.
Very rarely, cancer occurs in other cells in the cervix.
Risk factors
Risk factors for cervical cancer
include:
- Many sexual partners. The
greater your number of sexual partners — and the greater your partner's
number of sexual partners — the greater your chance of acquiring HPV.
- Early sexual activity. Having
sex at an early age increases your risk of HPV.
- Other sexually transmitted infections
(STIs). Having
other STIs — such as chlamydia, gonorrhea, syphilis, and HIV/AIDS — increases your risk of HPV.
- A weakened immune system. You may
be more likely to develop cervical cancer if your immune system is
weakened by another health condition and you have HPV.
- Smoking. Smoking
is associated with squamous cell cervical cancer.
- Exposure to miscarriage prevention
drugs. If your
mother took a drug called diethylstilbestrol (DES) while pregnant in the
1950s, you may have an increased risk of a certain type of cervical cancer
called clear cell adenocarcinoma.
Prevention
To reduce your risk of cervical cancer:
- Ask
your doctor about the HPV vaccine. Receiving
a vaccination to prevent HPV infection may reduce your risk of
cervical cancer and other HPV-related cancers. Ask your doctor
whether an HPV vaccine is appropriate for you.
- Have routine Pap tests. Pap
tests can detect precancerous conditions of the cervix, so they can be
monitored or treated to prevent cervical cancer. Most medical
organizations suggest beginning routine Pap tests at age 21 and repeating
them every few years.
- Practice safe sex. Reduce
your risk of cervical cancer by taking measures to prevent sexually
transmitted infections, such as using a condom every time you have sex and
limiting the number of sexual partners you have.
- Don't smoke. If you
don't smoke, don't start. If you do smoke, talk to your doctor about
strategies to help you quit.
Diagnosis
Screening
Screening tests can help detect
cervical cancer and precancerous cells that may one day develop into cervical
cancer. Most guidelines suggest beginning screening for cervical cancer and
precancerous changes at age 21.
Screening tests include:
Pap test.
A Pap test can detect abnormal cells in
the cervix, including cancer cells and cells that show changes that increase
the risk of cervical cancer.
HPV DNA test.
Discuss your cervical cancer screening
options with your doctor.
If cervical cancer is suspected, your
doctor is likely to start with a thorough examination of your cervix. A special
magnifying instrument (colposcope) is used to check for abnormal cells.
During the colposcopic examination,
your doctor is likely to take a sample of cervical cells (biopsy) for
laboratory testing. To obtain tissue, your doctor may use:
Punch biopsy,
Endocervical curettage
If the punch biopsy or endocervical
curettage is worrisome, your doctor may perform one of the following tests:
An electrical wire loop
Cone biopsy (conization),
Is a procedure that allows your doctor to obtain deeper layers of cervical cells for laboratory testing. A cone biopsy may be done in a hospital under general anesthesia.
Staging
If your doctor determines that you have
cervical cancer, you'll have further tests to determine the extent (stage) of
your cancer. Your cancer stage is a key factor in deciding on your treatment.
Staging exams include:
- Imaging tests. Tests
such as X-rays, CTs, MRIs, and positron emission tomography
(PET) help your doctor determine whether your cancer has spread beyond
your cervix.
- Visual examination of your bladder and
rectum. Your
doctor may use special scopes to see inside your bladder and rectum.
Treatment
Treatment for cervical cancer depends
on several factors, such as the stage of cancer, other health problems you
may have, and your preferences. Surgery, radiation, chemotherapy, or a
combination of the three may be used.
Surgery
Early-stage cervical cancer is
typically treated with surgery. Which operation is best for you will depend on
the size of your cancer, its stage, and whether you would like to consider
becoming pregnant in the future.
Options might include:
- Surgery to cut away cancer only. For very small cervical cancer, it might be possible to remove the cancer
entirely with a cone biopsy. This procedure involves cutting away a
cone-shaped piece of cervical tissue but leaving the rest of the cervix
intact. This option may make it possible for you to consider becoming
pregnant in the future.
- Surgery to remove the cervix
(trachelectomy). Early-stage
cervical cancer might be treated with a radical trachelectomy procedure,
which removes the cervix and some surrounding tissue. The uterus remains
after this procedure, so it may be possible to become pregnant if you
choose.
-
Surgery to remove the cervix and uterus (hysterectomy). Most early-stage cervical cancers are treated with a radical hysterectomy operation, which involves removing the cervix, uterus, part of the lady parts, and nearby lymph nodes. A hysterectomy can cure early-stage cervical cancer and prevent a recurrence. But removing the uterus makes it impossible to become pregnant.
Minimally invasive hysterectomy, which
involves making several small incisions in the abdomen rather than one large
incision, may be an option for early-stage cervical cancer. People who undergo
minimally invasive surgery tend to recover more quickly and spend less time in
the hospital. But some research has found minimally invasive hysterectomy may
be less effective than traditional hysterectomy. If you're considering
minimally invasive surgery, discuss the benefits and risks of this approach
with your surgeon.
Radiation
Radiation therapy uses high-powered
energy beams, such as X-rays or protons, to kill cancer cells. Radiation
therapy is often combined with chemotherapy as the primary treatment for
locally advanced cervical cancers. It can also be used after surgery if there's
an increased risk that cancer will come back.
Radiation therapy can be given:
- Externally,
by directing a radiation beam at the affected area of the body (external
beam radiation therapy)
- Internally,
by placing a device filled with radioactive material inside your vagina,
usually for only a few minutes (brachytherapy)
- Both
externally and internally
If you haven't started menopause yet,
radiation therapy might cause menopause. If you might want to consider becoming
pregnant after radiation treatment, ask your doctor about ways to preserve your
eggs before treatment starts.
Chemotherapy
Chemotherapy is a drug treatment that
uses chemicals to kill cancer cells. It can be given through a vein or taken in
pill form. Sometimes both methods are used.
For locally advanced cervical cancer,
low doses of chemotherapy are often combined with radiation therapy, since
chemotherapy may enhance the effects of the radiation. Higher doses of
chemotherapy might be recommended to help control symptoms of very advanced
cancer.
Targeted therapy
Targeted drug treatments focus on
specific weaknesses present within cancer cells. By blocking these weaknesses,
targeted drug treatments can cause cancer cells to die. Targeted drug therapy
is usually combined with chemotherapy. It might be an option for advanced
cervical cancer.
Immunotherapy
Immunotherapy is a drug treatment that
helps your immune system to fight cancer. Your body's disease-fighting immune
system might not attack cancer because the cancer cells produce proteins that
make them undetectable by the immune system cells. Immunotherapy works by
interfering with that process. For cervical cancer, immunotherapy might be
considered when the cancer is advanced and other treatments aren't working.
Supportive (palliative) care
Palliative care is specialized medical
care that focuses on providing relief from pain and other symptoms of a serious
illness. Palliative care specialists work with you, your family, and your other
doctors to provide an extra layer of support that complements your ongoing
care.
When palliative care is used along with
all of the other appropriate treatments, people with cancer may feel better and
live longer.
Palliative care is provided by a team
of doctors, nurses, and other specially trained professionals. Palliative care
teams aim to improve the quality of life for people with cancer and their
families. This form of care is offered alongside curative or other treatments
you may be receiving.
( Keywords )



Post a Comment